High blood pressure, or hypertension, is like a silent troublemaker in your body. It sneaks up, puts extra stress on your heart and blood vessels, and increases your risk for serious issues like heart attacks and strokes. One simple way to tackle it is by eating less salt. But what exactly happens to your blood pressure if you cut back on salt for 21 days? In this article, we’ll explore the science behind salt and blood pressure, look at what studies say, and give you practical tips to make it work—all in simple and plain English. We’re only using trusted sources to keep things reliable.
Why Does Salt Affect Your Blood Pressure?
Let’s start with the basics. Salt, or sodium chloride, is something your body needs to function. It helps balance fluids, keeps your nerves firing, and supports muscle movement. But too much salt can mess with your blood pressure. Here’s how it works:
When you eat salty foods, the sodium gets into your bloodstream. Your body likes to keep sodium levels steady, so it holds onto extra water to dilute it. This extra water increases the amount of blood in your veins and arteries, which raises the pressure against their walls—hello, high blood pressure! Over time, this extra pressure can make your blood vessels stiff and put your heart under strain.

The Centers for Disease Control and Prevention (CDC) says most Americans eat way too much sodium—about 3,400 mg a day, when the recommended limit is 2,300 mg (that’s about one teaspoon of salt, or 5.8 grams). If you have high blood pressure, doctors often suggest going even lower, to 1,500 mg (about 3.8 grams of salt). Cutting back on salt reduces the water your body holds, lowers blood volume, and eases that pressure on your blood vessels.
The Role of Your Kidneys
Your kidneys are like the body’s water managers. They filter your blood and decide how much water and sodium to keep or get rid of. When you eat a lot of salt, your kidneys hold onto more water to balance the sodium, which increases blood volume. If you cut salt, your kidneys can release more sodium and water, reducing blood volume and lowering blood pressure. The National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK) explains that this process is key to why salt reduction works for blood pressure control.
Other Factors at Play
It’s not just about water. High sodium levels can also make your blood vessels less flexible, which makes it harder for them to expand and contract. This stiffness adds to the pressure. Plus, sodium can affect hormones like aldosterone, which controls how much sodium and water your body keeps. Less salt means less aldosterone, which helps lower blood pressure, according to research from PubMed.
What Happens After 21 Days of Cutting Salt?
Now, let’s get to the big question: what changes can you expect in your blood pressure after 21 days of eating less salt? While not every study looks exactly at the 21-day mark, there’s plenty of evidence from older and newer research to give us a clear picture. Let’s break it down.
Early Evidence from 1904
Way back in 1904, two doctors named Ambard and Beaujard did a small but groundbreaking study. They had six patients with high blood pressure follow a low-salt diet for three weeks—exactly 21 days. As described in a review on Dietary Salt Intake and Hypertension, these patients saw their blood pressure drop during that time. This study was tiny and didn’t use modern methods, but it’s one of the earliest clues that cutting salt can lower blood pressure in just a few weeks, especially for people with hypertension.
Modern Studies: The DASH-Sodium Trial
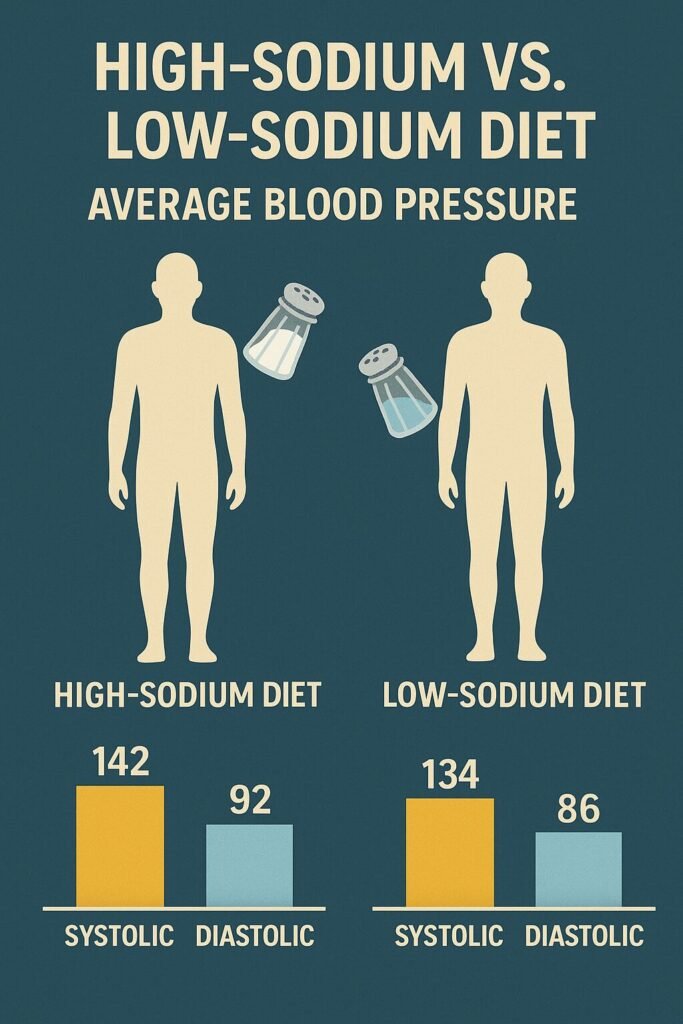
Fast forward to the year 2000, when the Dietary Approaches to Stop Hypertension (DASH)-Sodium trial gave us some solid data. Published in the New England Journal of Medicine and available on PubMed, this study involved 412 people with pre-hypertension or stage 1 hypertension. They ate at three sodium levels—high (3,300 mg/day), medium (2,400 mg/day), and low (1,500 mg/day)—for four weeks each.
Those on the low-sodium diet saw their blood pressure drop steadily over the four weeks, with an average weekly reduction of about 0.94 mm Hg systolic (the top number) and 0.70 mm Hg diastolic (the bottom number) compared to the high-sodium group.
By 21 days (three weeks), this adds up to an estimated drop of 2.82 mm Hg systolic and 2.10 mm Hg diastolic. If you have high blood pressure, the effect was even bigger—closer to 4 mm Hg systolic in some cases. This shows that 21 days is enough time to see real changes, especially if your blood pressure is already high.
2013 Meta-Analysis: Bigger Picture
A 2013 meta-analysis by He and MacGregor, published in The BMJ and found on PubMed, looked at 34 studies with over 3,230 participants. These studies tested modest salt reductions (about 4.4 grams of salt less per day) for at least four weeks. Across all participants, blood pressure dropped by an average of 4.18 mm Hg systolic and 2.06 mm Hg diastolic. For people with hypertension, the reductions were bigger: 5.39 mm Hg systolic and 2.82 mm Hg diastolic.
While these studies lasted at least four weeks, the researchers noted that blood pressure often starts dropping within the first week and keeps improving. This suggests that by 21 days, you could see reductions close to 2.8–5.4 mm Hg systolic and 2.1–2.8 mm Hg diastolic if you have high blood pressure, and slightly smaller drops (1–2 mm Hg systolic) if your blood pressure is normal.
2023 Study: Fast Results in One Week
A newer study from 2023, supported by the National Heart, Lung, and Blood Institute (NHLBI) and published in JAMA (PubMed), showed that cutting sodium to just 500 mg/day for one week lowered systolic blood pressure by 8 mm Hg compared to a high-sodium diet. This study included 213 people aged 50–75, some with normal blood pressure, some with hypertension, and some on blood pressure meds. The fact that such a big drop happened in just one week is exciting—it means that by 21 days, the effect could be even more significant, especially for those who are sensitive to salt.

Putting It All Together
Here’s a quick summary of what studies tell us about blood pressure changes after 21 days of reducing salt:
| Study/Source | Duration | Salt Reduction | Systolic BP Reduction (mm Hg) | Diastolic BP Reduction (mm Hg) | Notes |
|---|---|---|---|---|---|
| Ambard & Beaujard (1904) | 21 days | Not specified | Observed decrease | Observed decrease | Small study, hypertensives only |
| DASH-Sodium (2001) | 4 weeks | ~1,500 mg/day sodium | ~2.82 (estimated at 21 days) | ~2.10 (estimated at 21 days) | Bigger effect in hypertensives |
| 2013 Meta-Analysis | ≥4 weeks | 4.4 g/day salt | 4.18 (5.39 in hypertensives) | 2.06 (2.82 in hypertensives) | Effects start early, grow over time |
| 2023 NHLBI Study | 1 week | 500 mg/day sodium | 8 | Not specified | Suggests rapid, ongoing benefits |
For people with high blood pressure, cutting salt by 4–5 grams a day could lower systolic blood pressure by 2.8–5.4 mm Hg and diastolic by 2.1–2.8 mm Hg after 21 days. If your blood pressure is normal, expect smaller drops, around 1–2 mm Hg systolic and 0.5–1 mm Hg diastolic. These changes might not sound huge, but even a 2 mm Hg drop can lower your risk of heart disease over time, according to the CDC.
Who Sees the Biggest Benefits?
Not everyone reacts to salt the same way. Some people are “salt-sensitive,” meaning their blood pressure changes a lot when they eat more or less salt. Others are less sensitive, so their blood pressure stays pretty stable. The National Institutes of Health (NIH) says you’re more likely to be salt-sensitive if you:
- Have High Blood Pressure: People with hypertension see bigger drops (e.g., 5.39 mm Hg systolic vs. 2.42 mm Hg for normotensives in the 2013 meta-analysis).
- Are Older: As you age, your kidneys get less efficient at handling sodium, making you more salt-sensitive.
- Are African American: Studies like DASH-Sodium show this group often benefits more from salt reduction.
- Have Certain Genes: Some genetic factors make your blood pressure more responsive to salt, as noted in PubMed.
- Have Kidney Issues or Diabetes: These conditions can make your body hold onto sodium more, increasing salt sensitivity.
If you fit into one of these groups, cutting salt for 21 days is likely to make a noticeable difference in your blood pressure. Even if you’re not salt-sensitive, reducing salt can still help, just maybe not as dramatically.
How Much Salt Should You Cut?
So, how much salt should you aim for? The CDC recommends no more than 2,300 mg of sodium per day (5.8 grams of salt, or about one teaspoon). If you have high blood pressure, the American Heart Association, cited by the NHLBI, suggests 1,500 mg (3.8 grams of salt). Studies showing blood pressure drops often involve bigger cuts, like reducing salt by 4.4 grams a day or going as low as 500 mg sodium daily. Here’s what that looks like:
- Average Intake: Many people eat 10–12 grams of salt a day (4,000–4,800 mg sodium).
- Moderate Cut: Dropping to 5–6 grams of salt (2,000–2,400 mg sodium) aligns with WHO and CDC guidelines and can lower blood pressure.
- Bigger Cut: Aiming for 1,500 mg sodium (3.8 grams of salt) or less, like in the DASH-Sodium trial, may give bigger benefits, especially for hypertensives.
To put this in perspective, one teaspoon of salt is 5.8 grams, so cutting to 3.8 grams is about two-thirds of a teaspoon. It’s doable, but it takes some effort since most sodium comes from processed foods, not the salt you sprinkle on at home.
The Science of How Your Body Adjusts
When you start eating less salt, your body doesn’t just flip a switch—it goes through a series of adjustments. Here’s what happens over those 21 days, based on research like Sodium Intake and Hypertension:
- Days 1–3: Your kidneys start excreting more sodium and water, reducing blood volume slightly. You might notice you’re peeing more as your body gets rid of the extra fluid. Blood pressure may begin to drop, especially if you’re salt-sensitive.
- Days 4–7: Your blood vessels start to relax as sodium levels in your blood decrease. Hormones like aldosterone, which make you hold onto sodium, drop, helping lower blood pressure further. Studies like the 2023 NHLBI trial show significant drops (up to 8 mm Hg systolic) in this timeframe.
- Days 8–14: Your body continues adjusting, fine-tuning how it handles sodium. Blood pressure reductions become more stable, and you might notice less puffiness or swelling if you were retaining water before.
- Days 15–21: By now, your body has adapted to the lower sodium intake. Blood pressure reductions are more consistent, and your taste buds start getting used to less salty flavors. The DASH-Sodium trial suggests progressive improvements, with estimated drops of 2.8–5.4 mm Hg systolic by this point for hypertensives.
These changes aren’t just about blood pressure. Less sodium can also reduce strain on your heart, improve kidney function, and lower your risk of long-term damage to your blood vessels.
Practical Tips to Cut Salt Without Losing Flavor
Cutting salt doesn’t mean your food has to taste boring. Here are some easy, practical ways to lower sodium while keeping your meals tasty, inspired by tips from the NHLBI:
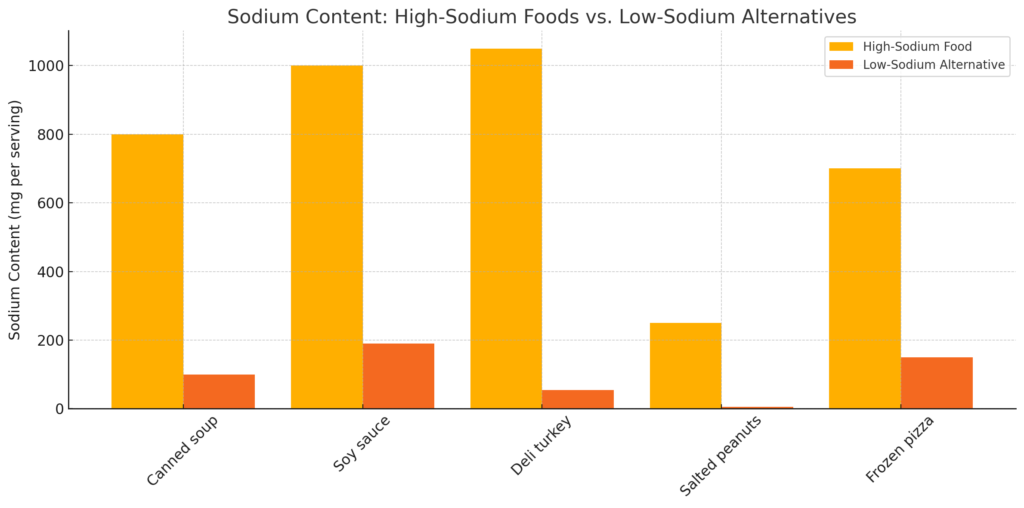
- Check Labels: Look for foods with less than 140 mg sodium per serving. Watch out for sneaky high-sodium items like canned soups, sauces, and frozen meals.
- Go Fresh: Fresh fruits, veggies, and unprocessed meats (like chicken or fish) are naturally low in sodium. Skip canned or frozen versions with added salt.
- Cook at Home: Making your own meals lets you control the salt. Flavor with herbs (basil, rosemary), spices (cumin, chili powder), or citrus (lemon, lime) instead.
- Rinse Canned Goods: If you use canned beans or veggies, rinse them under water to wash away extra sodium.
- Ditch Salty Snacks: Swap chips, pretzels, and crackers for fresh fruit, unsalted nuts, or air-popped popcorn.
- Be Condiment-Smart: Soy sauce, ketchup, and salad dressings can pack a sodium punch. Try low-sodium versions or make your own with vinegar and spices.
- Taste Before Salting: Get in the habit of tasting your food before reaching for the salt shaker. You might not need it!
- Stay Hydrated: Drinking plenty of water helps your kidneys flush out excess sodium.
It might take a week or two for your taste buds to adjust to less salt, but soon you’ll start appreciating the natural flavors of food. The CDC also suggests eating more potassium-rich foods (like bananas, spinach, and sweet potatoes), which can help balance sodium and lower blood pressure.
Challenges and Possible Side Effects
Reducing salt isn’t always a walk in the park. About 75% of the sodium we eat comes from processed and restaurant foods, not the salt we add at home, according to the FDA. This means you’ll need to rethink your grocery list and dining habits. Here are some challenges and how to handle them:
- Taste Adjustment: Food might taste bland at first. Try new spices or herbs to keep things exciting.
- Convenience: Processed foods are quick and easy, but they’re sodium bombs. Plan simple home-cooked meals, like grilled chicken with veggies, to save time.
- Eating Out: Restaurant meals are often loaded with salt. Ask for sauces on the side or choose grilled or steamed dishes.
Some studies, like one reviewed in Sodium Intake and Hypertension, suggest that very low sodium levels (below 2 grams/day) might increase risks like heart problems in some people with normal blood pressure. However, this is controversial, and most experts agree that cutting to 5–6 grams of salt a day is safe and beneficial for most people. If you’re on blood pressure meds or have health conditions, talk to your doctor before making big changes.
Controversies and Debates
While most scientists agree that reducing salt helps lower blood pressure, there’s some debate about how much it benefits people with normal blood pressure. A few studies, like those discussed in PubMed, argue that salt reduction has smaller effects in normotensive people and might not be worth the effort for everyone. However, the World Health Organization and CDC still recommend population-wide salt reduction because even small blood pressure drops can reduce heart disease risk across a large group.
Another debate is about very low sodium diets. Some researchers worry that dropping sodium too low could affect hormone levels or kidney function in certain people. But for most, sticking to 1,500–2,300 mg sodium daily is a safe bet, as supported by the NHLBI.
Why 21 Days Matters
The 21-day mark is interesting because it’s long enough for your body to adjust to less salt but short enough to feel achievable. By three weeks, your kidneys, blood vessels, and hormones have had time to adapt, and your blood pressure is likely showing measurable improvements. Plus, your taste buds are starting to get used to lower-sodium foods, making it easier to stick with the habit. The NIH notes that these changes can set the stage for long-term heart health benefits.
Conclusion
Cutting back on salt for 21 days can make a real difference in your blood pressure, especially if you have hypertension or are salt-sensitive. Studies, from a 1904 experiment to modern trials like DASH-Sodium and a 2023 NHLBI study, show that reducing salt by 4–5 grams a day can lower systolic blood pressure by 2.8–5.4 mm Hg and diastolic by 2.1–2.8 mm Hg in hypertensives by this time. Even if your blood pressure is normal, you might see smaller drops of 1–2 mm Hg. These changes come from your body holding less water, your blood vessels relaxing, and your kidneys working more efficiently.
By making simple swaps—like choosing fresh foods, cooking at home, and using herbs instead of salt—you can lower your sodium intake without sacrificing flavor. While it takes some effort to avoid processed foods and adjust your taste buds, the benefits for your heart and overall health are worth it. If you’re ready to try it, talk to your doctor, grab some fresh ingredients, and start your 21-day journey to better blood pressure!